The incidence of HIV and TB has contributed to the death of thousands of people annually across the world. The fight against these diseases has been at the core of many donor-funded programs in Lower- and Middle-income Countries (LMICs), and Nigeria like many other LMICs is no different. These programs – implemented as stand-alone health programs – have been instrumental in addressing key public health challenges in Nigeria. While the donor-funded vertical interventions bring immediate succor to public health concerns in the management of Malaria, TB and, HIV/AIDS, they are likely to fragment the health system, duplicate efforts, and often result in lack of local ownership of interventions caused by donor dependence; this ultimately makes prospects for sustainability bleak.
Like other states in Nigeria, Kaduna State’s HIV and  TB services are donor-funded and are currently assessed at no cost in public facilities. However, continuity of this may not be assured as donor funding ceases. In this light, inclusion of these programs as part of the health insurance benefit package to be publicly funded through pooled resources has become imperative. Integrating vertical programs into social health insurance schemes provides an opportunity for the government to take ownership of providing these services to its people and also ensures the sustainability of the programs post-donor funding. With Management Sciences for Health (MSH) as the Principal Recipient, HSCL as the Technical Service Organization (TSO) through the
TB services are donor-funded and are currently assessed at no cost in public facilities. However, continuity of this may not be assured as donor funding ceases. In this light, inclusion of these programs as part of the health insurance benefit package to be publicly funded through pooled resources has become imperative. Integrating vertical programs into social health insurance schemes provides an opportunity for the government to take ownership of providing these services to its people and also ensures the sustainability of the programs post-donor funding. With Management Sciences for Health (MSH) as the Principal Recipient, HSCL as the Technical Service Organization (TSO) through the  Global Fund Resilient and Sustainable Systems for Health (RSSH) Project conducted an actuarial costing of HIV and TB services as the first step towards achieving programs’ integration. The aim of the actuarial study was to determine the cost implication of including HIV and TB services in the state’s contributory health insurance benefit package by computing the disease burden in the state (using the service utilization data) and the cost of providing the treatment.
Global Fund Resilient and Sustainable Systems for Health (RSSH) Project conducted an actuarial costing of HIV and TB services as the first step towards achieving programs’ integration. The aim of the actuarial study was to determine the cost implication of including HIV and TB services in the state’s contributory health insurance benefit package by computing the disease burden in the state (using the service utilization data) and the cost of providing the treatment.
Prior to this actuarial study, HSCL conducted a benchmark study, identifying challenges and mitigation strategies from 3 countries, Kenya, Malawi and Cambodia. Like Nigeria, these countries have similar GDP per capita, HIV/AIDS, and TB prevalence rates; they also share the risks of running into deficit, poor service utilization, and implementation, which is faced by the integration process. Despite the similarities on these parameters among these three countries, the benchmark results have however shown that there is no standard method of integrating these services into the insurance scheme – the case studies showed that incremental integration processes have proven efficient for integration of TB and HIV/AIDS services into the health insurance scheme.
Following the benchmark study, HSCL began the actuarial study by analyzing and identifying key inclusion and exclusion criteria, which would serve as determinants of the outcome (See figure 1 below). HSCL developed a data collection tool and trained data enumerators to obtain the approved information required for the analysis. The information required, determined agencies with which HSCL engaged to obtain data. Components including population distribution (by age) and service utilization rates were obtained from agencies of the state including Kaduna State AIDS Control Agency (KADSACA), the Tuberculosis and Leprosy Control (TBL) Unit, State Ministry of Health (SMoH), and Kaduna Contributory Health Management Authority (KADCHMA), while the cost of health care services and commodities were obtained from Global Fund’s Pooled Procurement Mechanisms reference pricing and the Stop TB Partnership's Global Drug Facility. It is imperative to note that there were limitations to the study such as the inability to monitor trends and the impact of new diseases or interventions, and lack of clarity on funding mechanisms. As a result, certain assumptions were made before the study however; a database with granular details of information to be collected to support proper monitoring and future actuarial studies was developed and proposed to the State.
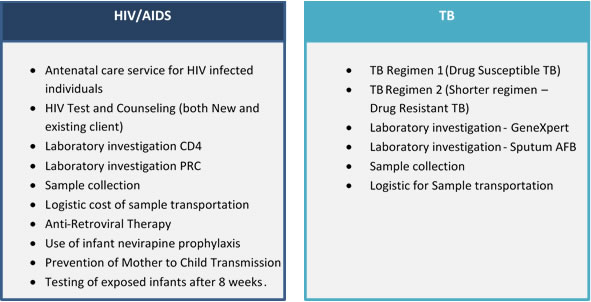
The actuarial study determined the cost of service provision, laboratory tests, and supply of required health commodities. Utilization rates and unit costs were derived to obtain the cost implication for HIV/AIDS and TB services. Findings from the actuarial studies show that the incremental cost of including HIV and TB services into the state’s benefit package will account for an additional 6.6% and 3.7% of the annual premium respectively.
In collaboration with Kaduna state, donors and development partners, HSCL will continue to provide technical assistance that focuses on generating data for decision-making processes from – but not limited to – pilot studies, facility assessments and capacity audits to ensure efficient and sustainable integration of HIV and TB services into Kaduna State contributory health insurance scheme.





