Journal: Journal of Environmental Protection (JEP)
Publisher: Scientific Research Publishing
Maxwell Obubu1*, Nkata Chuku1, Alozie Ananaba1, Firdausi Umar Sadiq Sadiq2, Emmanuel Sambo1, Oluwatosin Kolade1, Tolulope Oyekanmi1, Kehinde Olaosebikan1, Oluwafemi Serrano3
1Health Systems Consult Limited (HSCL), Abuja, Nigeria.
2Bill and Melinda Gates Foundation, Abuja, Nigeria.
3Head of Operations, Lagos State Health Management Agency (LASHMA), Lagos State, Nigeria.
DOI: 10.4236/jep.2023.142008 PDF HTML XML 14 Downloads 72 Views
Abstract
Background: Waste generation and its disposal is an essential issue in the sustainability of the environment and the planet’s future. Waste management is essential across sectors, likewise the health sector. Therefore, there is a need to employ extra care and attention to handling waste generated from healthcare facilities to avoid the dangers of poor biomedical waste management. We carried out this study to examine the waste management practice in healthcare facilities in Lagos State. Methods: The study was a descriptive survey carried out in one-thousand two hundred and fifty-six (1256) healthcare facilities in Lagos State. Nine hundred sixty-nine (969) of these facilities are located in urban areas, while two hundred and eighty-seven (287) are rural. The facilities studied are government/public health facilities (15.45%), private-for-profit facilities (82.88%), NGOs, Mission/Faith-Based medical facilities (1.67%). The data collected were analyzed using descriptive statistics. Specifically, we utilized bar charts, frequency, and percentage. Result: The result shows that 98.4% (1236) of the studied facilities are registered with the Lagos State Waste Management Authority (LAWMA), while 1.6% (20) are not registered. 98.5% (191) of the 194 government-owned facilities, 98.5% (1025) of the 1041 private-for-profit facilities, and 98.2% (20) of the 21 NGOs/faith-based health facilities are registered with Lagos State Waste Management Authority. The result also shows that 94% of the healthcare facilities studied in Lagos State use color-coded waste bags to segregate waste at the point of origin. 58.7% of the facilities use red-colored bags, 33.3% use yellow-colored bags, 10.7% use black-colored bags, and 1.3% use brown biohazard bags for segregating Infectious waste. Also, 34.2% of the health facilities in Lagos state use red-colored bags, 36.9% use yellow-colored bags, 11% use black-colored bags, and 4.1% use brown-colored bags to segregate their hazardous waste. Conclusion: Some healthcare facilities in Lagos State do not follow the recommended guidelines for medical waste segregation. Waste generated is not appropriately segregated at the point of origin into the recommended colored bags/bins in some facilities. Thus, a policy and procedure regulating healthcare waste are mandatory. It is important to regularly train healthcare workers on proper waste management practices and encourage staff to read and apply WHO rules in managing healthcare waste. Healthcare personnel should realize that hazardous material is a potential cause of a public disaster.
Keywords
Waste Generation, Hospital Waste Management, Stakeholder Roles, Healthcare Facilities, Lagos State, Lagos Waste Management Authority
Share and Cite:
Obubu, M. , Chuku, N. , Ananaba, A. , Sadiq, F. , Sambo, E. , Kolade, O. , Oyekanmi, T. , Olaosebikan, K. and Serrano, O. (2023) Lagos State Hospital Waste Management Practices: A Descriptive Overview with Stakeholders’ Role and Key Recommendations. Journal of Environmental Protection, 14, 108-125. doi: 10.4236/jep.2023.142008.
1. Introduction
Waste generation is one of the earliest activities attributed to humans, documented for the first time in anthropological records of historical civilizations [1] . From the waste generated from hunting and gathering to the more complex and sophisticated waste generation patterns of this new millennium, waste generation has remained an integral part of society due to civilization’s industrialization and other human activities [2] . We define waste as any material lacking direct value to the user. The production of waste material is known as the waste stream and includes the entire variety of refuse generated during domestic, industrial, construction, and commercial processes [3] .
Like other industries and institutions, healthcare facilities also generate waste. Healthcare waste (HCW) is a by-product of healthcare activities, including infectious and non-infectious waste generated during the diagnosis, treatment, or immunization of human beings or animals, in research activities in these fields, or during the production or testing of biologicals [3] . According to WHO [4] , these comprise sharp objects such as blades, needles, and syringes: non-sharps, such as bandages, swabs, body parts, and blood; chemicals, such as disinfectants, solvents, and mercury; pharmaceuticals and radioactive materials. Additionally, contaminated pharmaceutical products, expired drugs, and vaccines constitute medical waste and must be appropriately disposed of [5] . Discarded items contaminated from use in the handling of pharmaceuticals are also parts of medical waste. These discarded items include masks, connecting tubing, bottles or boxes with residues, drug vials, and syringe bodies [5] .
Waste generation, its disposal, and management are essential for the sustainability of the environment, and the planet’s future, particularly as the complex components create more significant environmental pollution and make waste disposal and management more difficult [6] . Healthcare wastes hold higher priority in waste management due to their hazardous nature. According to Muluken et al. [7] , some parts of healthcare waste are considered the most hazardous and can affect human health and badly pollute the environment (See Figure 1). A working environment with unsafe healthcare waste management practices may result in exposure to infectious wastes by Healthcare workers, patients, and clients that could, in turn, create infection due to blood-borne pathogens [8] . According to Baaki et al. [9] , planning a hospital waste management system is complex and challenging since healthcare waste is unique and heterogeneous.
Over the years, biomedical wastes have increased due to the increase in size and number of healthcare facilities, the exponential rise in population, industrial and economic growth, urbanization, and disposable products in health facilities [10] . While most of these wastes are domestic or municipal wastes, a small percentage have pathogenic properties, posing a threat to human health and the environment [9] . Managing this waste stream composition remains a significant challenge, particularly in developing countries. The small portion of healthcare waste, which accounts for around 25% of total waste, could contaminate the entire waste stream if not adequately managed [11] . Inefficient waste practices increase the risk of the entire medical waste stream becoming infectious/hazardous, posing significant health and environmental risks and high disposal costs [12] [13] .
In Lagos state, efforts toward proper and safe management of hazardous healthcare waste are necessary as inadequate waste management practices are norms in most healthcare facilities [7] . According to the WHO [4] classification of hazardous healthcare waste, the various medical waste types are sharp, infectious, pathological, pharmaceutical, chemical, and radioactive (See Table 1).
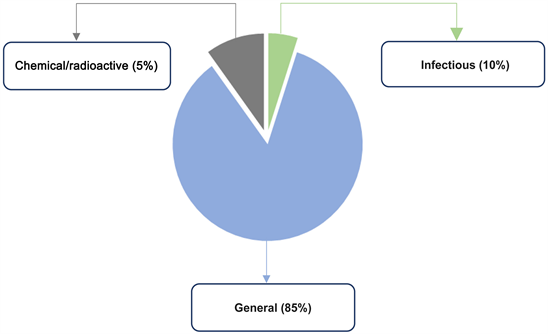
Figure 1. Typical waste compositions in healthcare facilities (Source: Safe management of wastes from healthcare activities, second edition).
| Waste category | Description and example |
|
Sharp Waste |
Used or unused sharps
e.g., hypodermic, intravenous, or other needles; auto-disable syringes; syringes with attached needles; infusion sets; scalpels; pipettes; knives; blades; broken glass. |
Infectious Waste |
Waste suspected to contain pathogens and pose a risk of disease transmission
e.g., waste contaminated with blood and other body fluids; laboratory cultures and microbiological stocks; waste including excreta and other materials that have been in contact with patients infected with highly infectious diseases in isolation wards. |
Pathological Waste |
Human tissues, organs or fluids; body parts; fetuses; unused blood products
Waste generated in any setting where tissue or blood specimens may be required for diagnostics or treatments e.g., organs, tissues, surgical specimens, bodily fluids removed during surgeries and autopsies. |
Pharmaceutical Waste |
Pharmaceuticals that are expired or no longer needed; items contaminated by or containing pharmaceuticals
Cytotoxic waste containing substances with genotoxic properties, e.g., waste containing cytostatic drugs (often used in cancer therapy); genotoxic chemicals |
Chemical Waste |
Waste containing chemical substances
e.g., laboratory reagents; film developer; disinfectants that are expired or no longer needed; solvents; waste with high heavy metal content, e.g., batteries; broken thermometers and blood pressure gauges |
Radioactive Waste |
Waste containing radioactive substances
e.g., unused liquids from radiotherapy or laboratory research; contaminated glassware, packages, or absorbent paper; urine and excreta from patients treated or tested with unsealed radionuclides; sealed sources |
Table 1. WHO classification of hazardous healthcare waste.
Waste contaminated with blood and its by-products, cultures, and stocks of infectious agents, waste from patients in isolation wards, discarded diagnostic samples containing blood and body fluids, infected animals from laboratories, and contaminated materials (swabs, bandages) and equipment (such as disposable medical devices); are considered as infectious waste. Pathological waste consists of organs, tissues, body parts, or fluids such as blood. Anatomical waste is a sub-group of pathological waste and consists of recognizable human body parts, whether infected or not [14] . These various types of medical waste are separated using a method called segregation.
Segregation separates different medical waste streams according to their classifications and is an essential part of the medical waste management process [9] . The essence is to separate infectious/hazardous waste from non-infectious/non-hazardous waste and prevent contamination [15] . Segregation would also reduce the quantity of infectious/hazardous waste. Segregation is more than just separating clinical waste from general medical waste, which determines the adoption of suitable treatment and disposal options [16] . Segregation should be through the use of color coding and labeling. Segregation at the time of waste generation is the medical staff’s sole responsibility [17] . Chartier et al. [11] suggested that all the waste generation points at healthcare facilities should have appropriate containers and bags matching the category of waste generated at each point of waste generation. According to [11] and the WHO recommended guidelines [4] , highly infectious waste should be in a yellow strong, leak-proof plastic bag or container capable of being autoclaved (see Table 2). This yellow bag should be marked ‘highly infectious’ with a biohazard symbol. Other infectious, pathological, and anatomical wastes should be placed in yellow-colored, leak-proof plastic bags or containers with a biohazard symbol. Sharp objects are to be placed in a yellow puncture-proof container marked “sharps” with a biohazard symbol. In addition to yellow, Lohani & Dixit [15] recommended red bags for infectious
| Type of waste | Colour of container | Type of container |
| Highly infectious waste | Yellow marked HIGHLY INFECTIOUS | Leak-proof and robust
plastic bag or container supporting autoclaving. |
| Other infectious waste, pathological and anatomic waste | Yellow | Leak-proof plastic bag or container |
| Sharps | Yellow marked SHARPS | Puncture-proof container |
| Chemical and pharmaceutical waste | Brown | Brown plastic bag or container |
| Radioactive waste | - | Lead box, labeled with the radioactive symbol |
| General healthcare waste | Black | Plastic bag |
Table 2. WHO recommended segregation and color coding for healthcare waste.
waste. Baaki et al. [9] suggested that pharmaceutical waste and chemicals be placed in a brown plastic bag (hospital-specific), while radioactive wastes should be placed in a lead box with the radioactive symbol. The general healthcare waste is to be placed in a black plastic bag.
Improper healthcare waste management as those seen in Figure 2, could results in infectious diseases, such as Hepatitis A, B, and HIV-2. WHO estimated that injections with contaminated syringes caused 21 million hepatitis B virus (HBV) infections (32% of all new infections), two million hepatitis C virus (HCV) infections (40% of all new infections), and 260,000 HIV infections (5% of all new infections) in the year 2000. In addition, healthcare activities generate significant amounts of hazardous waste such as mercury and expired pharmaceuticals and large amounts of general waste.
Today’s environment contends with global warming due to poor management of biodegradable and non-biodegradable solid waste [2] ; this is exacerbated by the astronomical rise in solid waste generation as a result of population and urbanization. Waste disposal is even more critical in today’s environment; existing trends of poor and irresponsible solid waste disposal are harmful to the environment and constitute a severe health danger to society [2] . Improper handling of medical waste can create harmful effects and reduce the overall benefits of healthcare. Studies by Olukanni et al. [18] and Uwa [5] in Nigeria show that medical waste management in Nigeria is poor, and general awareness of related issues is lacking among generators and handlers (Figure 1). It is, therefore, pertinent to assess the healthcare management practices in the healthcare facilities in Lagos State, Nigeria. The objectives of this study are to: 1) Ascertain if the healthcare facilities in Lagos State are registered with the state’s waste management authorities, 2) Examine the waste segregation methods employed by the healthcare facilities in Lagos State, 3) Examine stakeholders’ role in managing healthcare waste in Lagos State healthcare facilities, 4) Make critical recommendations for improving healthcare waste management.
![Figure 2. Hospital waste dumped indiscriminately at a tertiary health facility (Source: Uwa [5] ).](https://hscgroup.org/wp-content/uploads/2023/02/2.png)
Figure 2. Hospital waste dumped indiscriminately at a tertiary health facility (Source: Uwa [5] ).
2. Materials and Methods
2.1. Study Area; Size, Location, and Position
Lagos State is home to one of the world’s top twenty most populous cities. It is Africa’s largest city, with a population of approximately 21 million and a land area of 3577 km2. On the Southwestern coast of Nigeria, Lagos State geographically lies between Longitudes 2˚42'E and 3˚42'E and Latitudes 6˚22'N and 6˚52'N. Lagos State has five divisions: Ikeja, Badagry, Ikorodu, Lagos, and Epe. It segments into twenty (20) Local Government Areas (LGAs) and thirty-seven (37) Local Council Development Areas (LCDAs) for structured and comprehensive governance.
2.2. Lagos State Medical Waste Management
The Lagos Waste Management Authority (LAWMA) collects all waste from places categorized as public areas, namely: highways, major roads, streets, traditional markets, and other non-public areas such as households, schools, hospitals, construction sites, industries, shopping complexes, office blocks, hotels and so on. LAWMA Medical Waste Management Unit has been working jointly with the Lagos State Ministry of Health, the Hospital Facility Monitoring and Accreditation Agency (HEFAMAA), Lagos State Ministry of Environment, Lagos State Environmental Pollution Agency (LASEPA), and John Snow Incorporated (NGO). The joint initiative aims to develop a consistent regulatory approach to ensure proper management of hazardous waste generated at all healthcare facilities in Lagos State. Through this initiative, LAWMA Medical Waste Management Unit is developing strategies for addressing healthcare waste management concerns and achieving "best practice" regulatory compliances in all healthcare institutions.
Healthcare facilities produce various hazardous wastes, such as pharmaceuticals, chemotherapy, disinfectants, and mercury-containing wastes. When hazardous wastes are improperly treated, stored, transported, or disposed of, they can harm human health and the environment. LAWMA Medical Waste Management Unit is currently working with all hospitals in Lagos State, mainly public/general hospitals, to address their common problems regarding waste segregation from the point of generation and ensure compliance with hazardous waste requirements. For example, one common problem found in a couple of healthcare facilities audited in February and May 2008 is staff confusion about the different standards for managing hazardous and infectious waste. Hazardous waste is not the same as infectious waste (bio-hazardous, sharps, red bags, or regulated medical waste) and must be treated differently. Regarding this proposed initiative, LAWMA is also improving communications with healthcare facilities through various awareness programs, including an annual summit with stakeholders and quarterly interactive sessions to educate hospital staff on healthcare waste management and other problems hindering the program’s effectiveness. Figure 3 shows a healthcare waste collection exercise in a healthcare facility in Lagos State.

Figure 3. A healthcare waste collection exercise in a healthcare facility in Lagos state.
2.3. Data and Sampling Methods
The study used Universal Health Coverage data gathered while assessing health facilities in Lagos state (Obubu et al. [19] ). NOIPOLLSs carried out the health facility assessment with technical assistance from HSCL. NOIPOLLSs used a quantitative research methodology to assess health facilities, whereas HSCL compiled a list of health facilities using the State Ministry of Health data. The list served as a model for healthcare facilities in Lagos state. A census approach was used to select the sample frame of 2398 health facilities. NOIPoll remotely worked with key stakeholders to fine-tune the technical assistance plan for the health facility evaluation. The State Ministry of Health (SMOH), the Lagos State Health Insurance Agency (LASHMA), the Health Facility Monitoring and Accreditation Agency (HEFAMAA), and relevant professional bodies are among the stakeholders. s conducted telephone interviews with target respondents using Questionnaire Processing Software for Market Research (QPSMR). The final health facility assessment dataset includes information on facility ownership, facility level of care, accreditation status, human resources, essential medical and infection prevention equipment, infrastructure, available services, health insurance coverage, medicines and commodities, financial management systems, clinical governance, and Covid-19 response.
2.4. Statistical Method
The method of analysis employed in the study is descriptive statistics. We use bar charts, frequency, and percentages, to ascertain if the healthcare facilities in Lagos State are registered with waste management authorities and to examine the waste segregation methods employed by the healthcare facilities in Lagos State, Nigeria.
3. Results
3.1. Registration with LAWMA
The result in Figure 4 shows that 98.4% (1236) of the studied facilities are registered
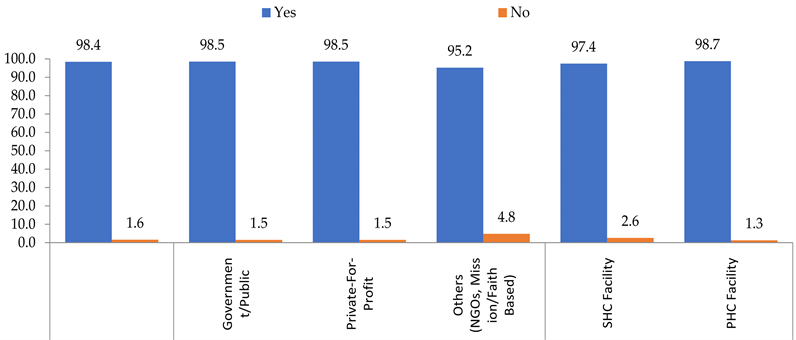
Figure 4. Healthcare facilities registered with LAWMA.
with the Lagos State Waste Management Authority (LAWMA), while 1.6% (20) are not registered. 98.5% (191) of the 194 government-owned facilities, 98.5% (1025) of the 1041 private-for-profit facilities, and 98.2% (20) of the 21 NGOs/faith-based health facilities are registered with Lagos State Waste Management Authority. The secondary healthcare facilities examined are 309; 301 (97.4%) have registration with LAWMA. Also, 98.7% (934) of the 946 primary facilities examined have registration with LAWMA.
3.2. Waste Segregation
As seen in Figure 5, 97.9% (1229) of the studied facilities segregate waste at the point of generation, while 2.1% (27) of them do not. The government-owned facilities that segregate waste at the time of collection are 96.9% (188), private 98.3% (1023), and NGOs/mission 85.7% (18). Primary healthcare facilities (98.2%) practice waste segregation at the time of collection more than the secondary healthcare facilities (96.8%).
3.3. Segregation Methods
Figure 6 shows that 94% of the healthcare facilities studied in Lagos State use color-coded waste containers as the segregation method for medical waste. 92.7%, 94.6%, and 76.2%, respectively, of public, private, and NGO/faith-based owned health facilities use color-coded waste containers for segregation at the time of waste collection. This result shows that the most widespread medical waste management practice in the healthcare facilities in Lagos is waste separation at the point of origin using color-coded waste containers.
3.4. Type of Waste and Color of Waste Segregation Bag
Infectious and pathological wastes are primarily packed in a red-colored bag, as
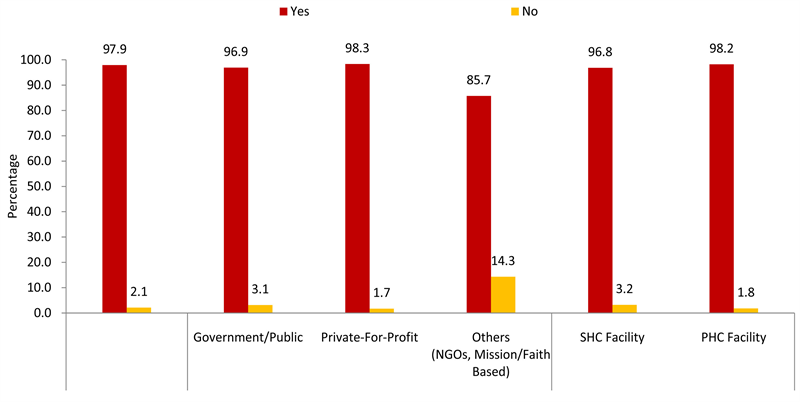
Figure 5. Percentage of HFs that practice Segregationof Wastes at the point of generation/time of collection.
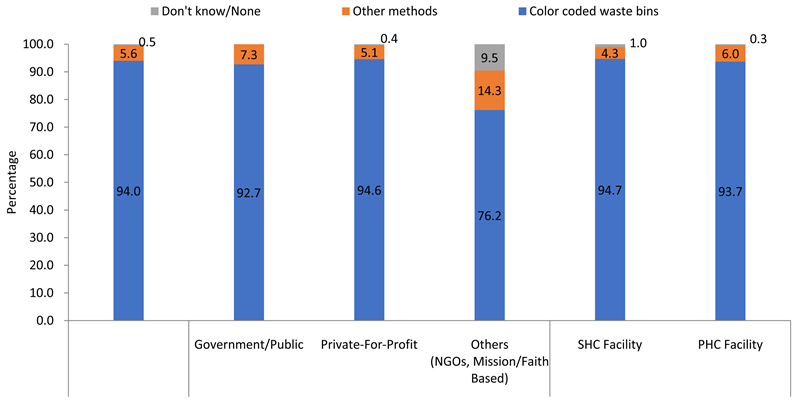
Figure 6. Percentage of facilities that uses waste segregation at the time of collection.
shown in Figure 7. 58.7% and 33.9% of the facilities store their infectious and pathological waste, respectively, in red-colored bags, and 34.2% of them equally store hazardous waste in a red-colored bag (Figure 5). 33.3% of the facilities use a yellow-colored bag for infectious waste, 36.9% use yellow for hazardous waste, and 17% for pathological waste. Black segregation bags are used by 10.7%, 11%, and 29.1% of healthcare facilities for infectious, hazardous, and pathological waste. Other colors used are brown, green, and purple (the least used).
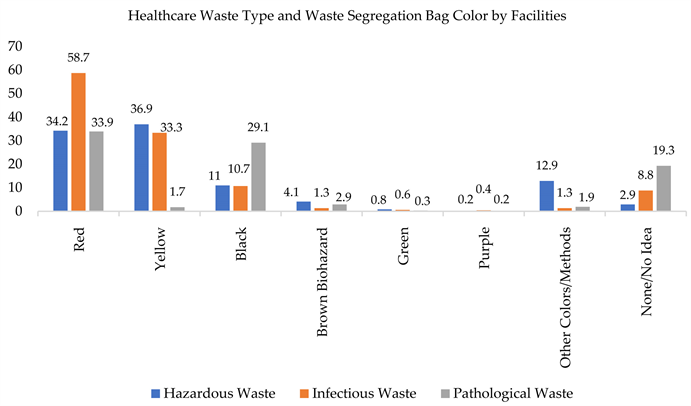
Figure 7. Type of waste and colour of waste segregation bag.
3.5. Storage of Sharp Waste by Healthcare Facilities
Sharp wastes are primarily stored in sharp or safety boxes, as shown in Figure 8, in which 89.7% of the facilities adopt this Method. 1.6% of the studied facilities use color-coded bags to store sharp waste, 3.7% use covered containers, and 1.6% use other waste storage methods. This is similar to findings by Attrah et al. (2022) [20] .
Table 3 shows that LAWMA medical waste, premium cleaners, and other waste management agencies dispose of sharp waste generated by 65.4% of the facilities in Lagos State. These agencies also dispose of the sharp waste generated by 36.8% of the facilities. The number of facilities that store sharp waste in a covered container is 88 (7%), and equally, 7% of the facilities store non-sharps in a covered container. 0.5% of the facilities dispose of their sharp waste by burning/burying it, and 1.7% burn/bury non-sharp waste. 0.5% of the facilities use 2 Chamber industrial (800 - 1000+ ˚C) Incinerators to dispose of sharp objects, and 0.3% of the facilities use is to dispose of non-sharps. 0.3% and 0.2% of the facilities use 1 Chamber drum/brick Incinerator to dispose of sharps and non-sharp waste.
4. Discussion
Waste management has been a severe challenge faced by developing countries. Medical waste, unlike other waste, requires special handling from the point they are generated to disposal, especially infectious ones. The study results show that 98.4% of the studied facilities are registered with the Lagos State Waste Management Agency (LAWMA). Various facility ownership type statistics show that 1.5%, 1.5%, and 4.8% of public, private-for-profit, and NGO/faith-based health facilities are not registered with LAWMA. Regarding the facility’s level of care,
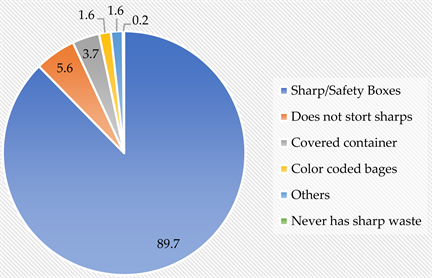
Figure 8. Storage of sharp waste by healthcare facilities.
| Method | Sharps | Non-sharps | ||
| Frequency | Percent | Frequency | Percent | |
| Same as for sharp items | 259 | 20.6 | 417 | 33.2 |
| 2 Chamber industrial (800 - 1000+ ˚C -Incinerator) | 6 | 0.5 | 4 | 0;3 |
| 1 Chamber drum/brick Incinerator | 4 | 0.3 | 3 | 0.2 |
| Flat ground no protection | 1 | 0.1 | 3 | 0.2 |
| Pit or protected ground | 4 | 0.3 | 2 | 0.2 |
| Covered pit or pit Latrine | 3 | 0.2 | 2 | 0.2 |
| Open pit-no protection | 0 | 0 | 1 | 0.1 |
| Protected ground or pit | 1 | 0.1 | 9 | 0.7 |
| Stored in a covered container | 88 | 7.0 | 88 | 7.0 |
| Stored in a protected environment | 23 | 1.8 | 37 | 2.9 |
| Stored unprotected | 4 | 0.3 | 3 | 0.2 |
| Never has sharp waste | 3 | 0.2 | 96 | 7.6 |
| Does not store sharps | 113 | 9.0 | 0 | 0 |
| Burnt and/or buried | 6 | 0.5 | 21 | 1.7 |
| Safety box | 5 | 0.4 | 0 | 0 |
| LAWMA Medical Waste/Premium Cleaners/Other Waste agencies | 709 | 65.4 | 462 | 36.8 |
| Don't know/Refused/Not applicable | 47 | 3.7 | 128 | 10.2 |
Table 3. Methods of waste disposal used by facilities in Lagos state.
2.6% of secondary and 1.3% of primary facilities are not registered with LAWMA, showing that waste disposal is handled internally by those facilities through burning is evidenced in Ola-Adisa et al. [2] .
One of the most important aspects of waste management in the medical sector is the segregation of waste [2] [11] . Findings revealed that 97.9% of the studied facilities segregate waste at the point of generation; this shows that many medical facilities practice waste segregation at the point of generation, as Lohani & Dixit [15] reported. However, some health facilities are still behind in this waste management practice. Poor waste management practices could be hazardous as infectious and non-infectious waste is mixed. This poses a severe threat to those handling them since there is no information on the type of waste in the waste container, and any careless contact could result in a life-threatening infection [15] [18] . Medical waste must be managed appropriately, as indiscriminate dumping or disposal of infectious/hazardous waste could cause a severe environmental hazard [12] .
Findings revealed that 94% of the facilities use color-coded waste containers as their Method of waste segregation at the point of origin, while 5.6% use other methods. In this study, the wastes are classified into three. The colors of bags/bins used in the studied facilities to separate these wastes at the time of collection are red, yellow, black, brown, green, and purple. 58.7% of the facilities use a red-colored container for infectious waste, 33.3% use yellow, 10.7% use black, and 1.3% use a brown biohazard bag. For hazardous waste, facilities using the red-colored bin are 34.2%, 36.9% use yellow, 11% use black, and 4.1% use brown. The result shows that more than one type of colored waste bag is used to segregate waste at the point of origin in the studied healthcare facilities. Yellow, as recommended by Baaki et al. [9] , Chartier et al. [11] , and WHO [17] , for infectious waste is used by 33.3% of the facilities, while red, in addition to yellow as recommended by Lohani & Dixit [15] , is used by 58.7% of the studied facilities. 10.7% of the facilities use black waste bins meant for general (non-infectious) waste to store infectious waste. 34.2% of healthcare facilities use red bags, and 36.9% use yellow bags to segregate hazardous waste at the point of origin [11] [15] . 11% of the facilities use black bags recommended for general waste to store hazardous waste. Findings revealed that 29.1% of the studied facilities use black-colored waste bags for pathological waste instead of the recommended red or yellow [9] [15] . The study’s findings also revealed that 89.8% of the facilities store sharp waste in sharp/safety boxes, as evidenced by Muluken et al. [7] .
Role of Stakeholders
Managing the various and interdependent facets of HCW at the facilities involves internal stakeholders such as all staff, patients, caregivers, and external stakeholders such as the government, policymakers, law enforcement authorities, waste management services providers, and academia. Table 4 shows an overview of the roles of stakeholders. Responsibilities with the authority and resources required to carry out steps involved in proper HCW management should be identified (Figure 9). However, the level of participation described below is achievable only through allocating resources and commitment at all levels. Besides, effective relations between government departments, the public,
| Stakeholders | Roles |
| Patients | Cooperate in complying with practices of healthcare waste management and, where possible, insist caretakers do so. |
| Patients’ families and caretakers | Cooperate in complying with healthcare waste management practices and, where possible, insist that nurses and laborers do so. |
| Healthcare workers | Carry out disease prevention duties (such as cleaning healthcare waste management) consistently and well.
Follow the rules for healthcare waste segregation. Inform patients and caretakers about in-house practices on waste management. Cooperate with management and participate actively in achieving and maintaining waste minimization targets. |
| Healthcare facility managers | Plan and implement healthcare waste management programs to set, achieve, monitor, and maintain targets.
Create incentives for staff and motivate them to meet and maintain targets Cooperate with top management, convince them and obtain support for healthcare waste management and recycling activities |
| Health authorities | Provide resources and direction for setting, achieving, and maintaining healthcare waste reduction targets
Publicize good practices of healthcare waste management and arrange for guided visits to poor-performing hospitals Coordinate peer group meetings to share results of better healthcare waste management practices |
| Academia | Raise awareness in medical schools and other sectors
Provide training for the health sector |
| Policymakers | Provide and mobilize political and financial support for improvements |
| National and International Funding bodies | Provide funding for new healthcare waste management programs |
Table 4. Role of stakeholders.
the private, and local communities are essential for effective and efficient HCW management in healthcare facilities. It could be established that the overall condition of HCW generation warrants immediate attention and action.
In order of importance, a synthesis of information from Lagos State illustrates three critical areas for immediate action (See Table 5). Healthcare waste management requires action by both governments and healthcare facilities. Lack of budget is a principal reason for ineffective healthcare waste management systems.
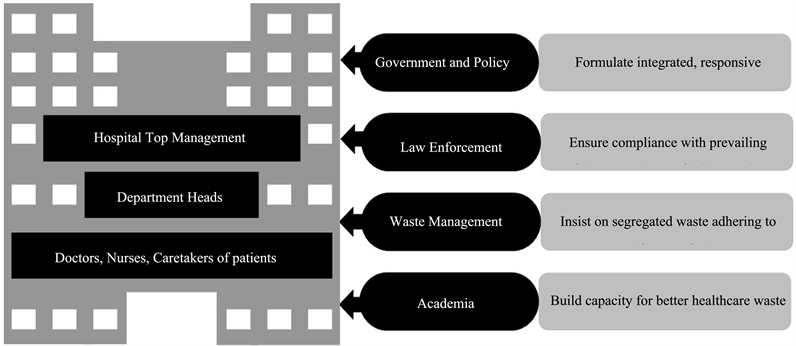
Figure 9. Distribution of responsibilities.
| Lagos State Government | Healthcare facility | |
| Budget |
|
|
| Policy and Legislation |
|
|
| Technology and knowledge management |
|
|
Table 5. Key recommendations for improving HCW management.
Governments lack the budget to implement waste treatment and disposal facilities, and healthcare facilities lack the budget to establish appropriate waste collection and handling services. The absence of enabling policies is one of the reasons for poor healthcare waste management. Such policies can be classified as internal and external policies. Internal policies are those established by the healthcare facility to demonstrate their commitment to better healthcare waste management, while external policies are those of the governments and regulatory authorities. Healthcare waste management includes technology and knowledge management—national governments and healthcare facilities often lack the required skills. To ensure better waste management, capacity building and training are required at appropriate levels for governments and healthcare facilities.
5. Conclusion
Waste management is essential in the health sector. Extra care and attention are required in handling waste generated from healthcare facilities to avoid the dangers or adverse effects of poor biomedical waste management. The study examines the waste management practice in healthcare facilities in Lagos State. Findings revealed that some healthcare facilities did not follow the recommended guidelines for medical waste segregation in Lagos State. Waste generated was not appropriately segregated at the point of origin into the recommended colored bags/bins in some facilities; this indicates that the waste management practice in some of the studied facilities is poor and could constitute a health risk for the staff. Though a more significant number of the studied facilities engaged the service of LAWMA Medical Waste, Premium Cleaners, and other waste agencies in disposing of the waste, some of the facilities preferred to bury them while some burn them. The medical staff feels the hazardous effect of burning medical waste in the facilities and neighborhood. This practice could be attributed to the lack of enforcement or implementation of biomedical waste management regulations and guidelines. It could be seen from the findings that some healthcare facilities are engaging in open incineration, which has adverse effects both on humans and the environment. Therefore, an improved method of waste management practice like using an autoclave to sterilize waste before final disposal, should be employed to ensure the safety of humans and the environment. Regular training of medical staff to improve waste management practice should be encouraged. Waste segregation at the point of origin is an ideal standard and should be encouraged. The recommended color-coded bags/boxes should be used to store the different types of waste.
Author Contributions
All authors contributed equally to the conception and design of the study.
Funding
This research is part of the work supported by the Bill and Melinda Gates Foundation (BMGF) through the Nigerian-led Strategic Purchasing for Family Planning grant [Grant Number: INV-007359] assigned to HSCL.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflict of Interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
References
1. WHO (2015) Lecture 5: Minimization, Recycling, and Segregation of HCW. World Health Organization, Geneva.
2. Ola-Adisa, E.O., Mangden, Y.E., Sati, Y.C. and Adisa, J.O. (2015) Knowledge, Attitudes/Beliefs and Practices in Medical Waste Management—An Appraisal of Jos North LGA, Plateau State, Nigeria. International Journal of Research in Humanities and Social Studies, 2, 43-56.
3. Babatola, J.O. (2018) A Study of Hospital Waste Generation and Management Practice in Akure, Nigeria. African Research Review, 2, 292-305.https://doi.org/10.4314/afrrev.v2i3.41074
4. WHO and Regional Office for the Western Pacific (2008) Workshop on Health Care Waste Management Planning and Implementation, Ulaanbaatar, Mongolia, 6-8 May 2008: Report.https://iris.wpro.who.int/bitstream/handle/10665.1/6256/RS_2008_GE_17_MOG_eng.pdf
5. Uwa, C.U. (2014) Assessment of Healthcare Waste Management Practices in Enugu Metropolis, Nigeria. International Journal of Environmental Science and Development, 5, 370-374. https://doi.org/10.7763/IJESD.2014.V5.512
6. Jatau, A.A. (2013) Knowledge, Attitudes, and Practices Associated with Waste Management in Jos South Metropolis, Plateau State. Mediterranean Journal of Social Sciences of Rome, 4, 119-121. https://doi.org/10.5901/mjss.2013.v4n5p119
7. Muluken, A., Haimanot, G. and Mesafint, M. (2013) Healthcare Waste Management Practices among Healthcare Workers in Healthcare Facilities of Gondar Town, Northwest Ethiopia. Health Service Journal, 12, 315-326.
8. Sawalem, M., Selic, E. and Herbell, J.D. (2009) Hospital Waste Management in Lybia: A Case Study. Waste Management, 29, 1370-375.https://doi.org/10.1016/j.wasman.2008.08.028
9. Baaki, T.K., Baharum, M.R. and Akashah, F.W. (2017) Critical Success Factors of Medical Waste Management Implementation in Healthcare Facilities in Nigeria: A Case Study. Journal of Design and Built Environment, 17, 18-35.https://doi.org/10.22452/jdbe.vol17no1.2
10. Mohee, R. (2005) Medical Wastes Characterization in Healthcare Institutions in Mauritius. Waste Management, 25, 575-581.https://doi.org/10.1016/j.wasman.2004.10.003
11. Chartier, Y., Emmanuel, J., Pieper, U., et al. (2014) Safe Management of Wastes from Healthcare Activities. 2nd Edition, World Health Organization, Geneva.
12. Coker, A., Sangodoyin, A., Sridhar, M., et al. (2009) Medical Waste Management in Ibadan, Nigeria: Obstacles and Prospects. Waste Management, 29, 804-811.https://doi.org/10.1016/j.wasman.2008.06.040
13. Nichols, A., Grose, J. and Mukonoweshuro, R. (2016) Achieving Cost and Carbon Savings in Neonatal Practice: A Review of the Literature on Sustainable Waste Management. Journal of Neonatal Nursing, 22, 81-87.https://doi.org/10.1016/j.jnn.2016.01.002
14. Nwachukwu, N.C., Orji, F.A. and Ugbogu, O.C. (2013) Health Care Waste Management—Public Health Benefits, and the Need for Effective Environmental Regulatory Surveillance in Federal Republic of Nigeria. In: Rodriguez-Morales, A.J., Ed., Current Topics in Public Health, IntechOpen, London, 149-178.https://doi.org/10.5772/53196
15. Lohani, N. and Dixit, S. (2017) Biomedical Waste Management Practices in a Tertiary Care Hospital: A Descriptive Study in Srinagar, Garhwal, India. International Journal of Community Medicine and Public Health, 4, 465-470.https://doi.org/10.18203/2394-6040.ijcmph20170274
16. Abor, P.A. and Bouwer, A. (2008) Medical Waste Management Practices in a Southern African Hospital. International Journal of Health Care Quality Assurance, 21, 356-364. https://doi.org/10.1108/09526860810880153
17. WHO (2005) Lecture 7: Safe Management of Waste for Healthcare Facilities. World Health Organization, Geneva.
18. Olukanni, D.O., Azuh, D.E., Toogun, T.O. and Okorie, U.E. (2017)Medical Waste Management Practices among Selected Healthcare Facilities in Nigeria. Scientific Research and Essays, 9, 431-439. https://doi.org/10.5897/SRE2014.5863
19. Obubu, M., Chukwu, N., Ananaba, A., Sadiq, F.U., Sambo, E., Kolade, O., et al. (2022) Lagos State Health Facility Assessment Tool. Figshare. https://doi.org/10.6084/m9.figshare.21778871.v1
20. Attrah, M., Elmanadely, A., Akter, D. and Rene, E.R. (2022) A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments, 9, Article No. 146. https://doi.org/10.3390/environments9110146
Conflicts of Interest
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
References
| [1] | WHO (2015) Lecture 5: Minimization, Recycling, and Segregation of HCW. World Health Organization, Geneva. |
| [2] | Ola-Adisa, E.O., Mangden, Y.E., Sati, Y.C. and Adisa, J.O. (2015) Knowledge, Attitudes/Beliefs and Practices in Medical Waste Management—An Appraisal of Jos North LGA, Plateau State, Nigeria. International Journal of Research in Humanities and Social Studies, 2, 43-56. |
| [3] | Babatola, J.O. (2018) A Study of Hospital Waste Generation and Management Practice in Akure, Nigeria. African Research Review, 2, 292-305. https://doi.org/10.4314/afrrev.v2i3.41074 |
| [4] | WHO and Regional Office for the Western Pacific (2008) Workshop on Health Care Waste Management Planning and Implementation, Ulaanbaatar, Mongolia, 6-8 May 2008: Report. https://iris.wpro.who.int/bitstream/handle/10665.1/6256/RS_2008_GE_17_MOG_eng.pdf |
| [5] | Uwa, C.U. (2014) Assessment of Healthcare Waste Management Practices in Enugu Metropolis, Nigeria. International Journal of Environmental Science and Development, 5, 370-374. https://doi.org/10.7763/IJESD.2014.V5.512 |
| [6] | Jatau, A.A. (2013) Knowledge, Attitudes, and Practices Associated with Waste Management in Jos South Metropolis, Plateau State. Mediterranean Journal of Social Sciences of Rome, 4, 119-121. https://doi.org/10.5901/mjss.2013.v4n5p119 |
| [7] | Muluken, A., Haimanot, G. and Mesafint, M. (2013) Healthcare Waste Management Practices among Healthcare Workers in Healthcare Facilities of Gondar Town, Northwest Ethiopia. Health Service Journal, 12, 315-326. |
| [8] | Sawalem, M., Selic, E. and Herbell, J.D. (2009) Hospital Waste Management in Lybia: A Case Study. Waste Management, 29, 1370-375. https://doi.org/10.1016/j.wasman.2008.08.028 |
| [9] | Baaki, T.K., Baharum, M.R. and Akashah, F.W. (2017) Critical Success Factors of Medical Waste Management Implementation in Healthcare Facilities in Nigeria: A Case Study. Journal of Design and Built Environment, 17, 18-35. https://doi.org/10.22452/jdbe.vol17no1.2 |
| [10] | Mohee, R. (2005) Medical Wastes Characterization in Healthcare Institutions in Mauritius. Waste Management, 25, 575-581. https://doi.org/10.1016/j.wasman.2004.10.003 |
| [11] | Chartier, Y., Emmanuel, J., Pieper, U., et al. (2014) Safe Management of Wastes from Healthcare Activities. 2nd Edition, World Health Organization, Geneva. |
| [12] | Coker, A., Sangodoyin, A., Sridhar, M., et al. (2009) Medical Waste Management in Ibadan, Nigeria: Obstacles and Prospects. Waste Management, 29, 804-811. https://doi.org/10.1016/j.wasman.2008.06.040 |
| [13] | Nichols, A., Grose, J. and Mukonoweshuro, R. (2016) Achieving Cost and Carbon Savings in Neonatal Practice: A Review of the Literature on Sustainable Waste Management. Journal of Neonatal Nursing, 22, 81-87. https://doi.org/10.1016/j.jnn.2016.01.002 |
| [14] | Nwachukwu, N.C., Orji, F.A. and Ugbogu, O.C. (2013) Health Care Waste Management—Public Health Benefits, and the Need for Effective Environmental Regulatory Surveillance in Federal Republic of Nigeria. In: Rodriguez-Morales, A.J., Ed., Current Topics in Public Health, IntechOpen, London, 149-178. https://doi.org/10.5772/53196 |
| [15] | Lohani, N. and Dixit, S. (2017) Biomedical Waste Management Practices in a Tertiary Care Hospital: A Descriptive Study in Srinagar, Garhwal, India. International Journal of Community Medicine and Public Health, 4, 465-470. https://doi.org/10.18203/2394-6040.ijcmph20170274 |
| [16] | Abor, P.A. and Bouwer, A. (2008) Medical Waste Management Practices in a Southern African Hospital. International Journal of Health Care Quality Assurance, 21, 356-364. https://doi.org/10.1108/09526860810880153 |
| [17] | WHO (2005) Lecture 7: Safe Management of Waste for Healthcare Facilities. World Health Organization, Geneva. |
| [18] | Olukanni, D.O., Azuh, D.E., Toogun, T.O. and Okorie, U.E. (2017)Medical Waste Management Practices among Selected Healthcare Facilities in Nigeria. Scientific Research and Essays, 9, 431-439. https://doi.org/10.5897/SRE2014.5863 |
| [19] | Obubu, M., Chukwu, N., Ananaba, A., Sadiq, F.U., Sambo, E., Kolade, O., et al. (2022) Lagos State Health Facility Assessment Tool. Figshare. https://doi.org/10.6084/m9.figshare.21778871.v1 |
| [20] | Attrah, M., Elmanadely, A., Akter, D. and Rene, E.R. (2022) A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments, 9, Article No. 146. https://doi.org/10.3390/environments9110146 |






